Cataract surgery is very successful. Removing a cataract and replacing it with a new artificial lens leads to a remarkable improvement in vision. But as quick as the recovery is after cataract surgery, it still isn’t instantaneous. And some individuals can notice some blurry vision after cataract surgery.
The vision will be blurry immediately after cataract surgery. Beyond that, the prescription of the eye or dry eye are the biggest causes of blurry vision after cataract surgery. There are also less common medical reasons such as swelling, infection, and even “after cataracts".
Lots to cover today, so let's break it down into a few different categories
- Blurry vision right after the surgery
- The very common reasons why vision can be blurry beyond that
- Less common medical reasons worth knowing about
- The severe causes of blurry vision
Right After The Surgery
Immediately after you get your cataracts taken out, there are a few reasons why everything can be blurry. I mean, you did just have surgery after-all. Fortunately all of this heals over within a day or two after cataract surgery.
Dilation
In order for the surgeon to remove the cataract, the eye must be dilated. This dilation will persist for about 4-6 hours after cataract surgery in most cases. Occasionally it can last just a little bit longer.
While the eyes are dilated, you will have some additional blurry vision (in addition to everything being brighter than normal). When the pupil is large, extra light can enter the eye. This light doesn't all focus perfectly within the eye. This creates symptoms of glare and halos which can cause your vision to be a little more blurry.
Irritation on the surface of the eye
On the very surface of the cornea is a thin layer of cells called epithelial cells. These cells protect and maintain the health of the rest of the cornea. When these cells are perfectly healthy, these cells are completely transparent allowing you to see. But this layer of cells get put through the wringer during cataract surgery.
First off, the main antiseptic used to prevent infection after cataract surgery is betadine. Works great to kill bacteria! But also technically toxic to the eye as well (but not toxic enough to override the anti-bacteria ability). This will irritate that epithelial layer and make it more cloudy.
On top of this, the eye can dry out more during cataract surgery. An eyelid holder is used to keep the eye open during the procedure. This prevents you from having to worry about holding your eyes open or blinking during the procedure. But blinking serves an essential role for the eyes. Blinking restores the natural tear film on the surface of your eye. Without blinking, this tear film dries up.
During cataract surgery, your tear film is drying up. Now, the surgeon will be constantly artificially restoring your tear film with drops or a thicker gel, but the eye will still dry out a little bit more than normal. This will also contribute to the epithelium becoming "sicker" and more cloudy after cataract surgery.
This will cause your vision to be more blurry and foggy after the procedure, but this mostly heals up after a good night's sleep.
Swelling of the cornea
On the opposite side of the epithelium on the cornea is another small layer of cells called endothelium. These cells have one role: pump extra water out of the cornea.
Endothelium on bottom of cornea; Image by StemBook (CC BY 3.0) / modified from original
The cornea sits right next to water (inside the eye). Thus, these cells are constantly working to pump out extra water that makes its way into the cornea.
Extra water that gets into the cornea can cause it to swell. This swelling will alter the transparent structures of the cornea causing things to be more cloudy. This swelling will also change the way the cornea focuses light also causing things to be a little more blurry.
During cataract surgery two things happen.
- Through a process called phacoemulsification, a special instrument uses ultrasound waves to break up the cataract. These ultrasound waves if applied close to unprotected endothelial cells can "stun" or even damage those endothelial cells and prevent them from pumping water out of the cornea.
- Because the eye is a liquid-based environment, cataract surgery is performed completely "under water" so to speak. Because a tiny vacuum is used, water that is removed must be replaced with new water via irrigation. Sometimes this irrigation can push extra water into the cornea causing more swelling. (this is especially the case with the tiny cataract incisions - water is intentionally used to cause some swelling and close cataract incisions without sutures).
Between extra water pushed into the cornea and the endothelial cells becoming impaired, swelling can build up in the cornea.
Anticipating this, cataract surgeons place a thick gel coating over the endothelial cells to protect them and limit the swelling after cataract surgery. And this works very well; with most cataracts, there isn't much swelling. But very dense cataracts (and especially if special medication is used to visualize the dense cataract) can lead to a much higher amount of swelling after cataract surgery.
Depending on the amount of swelling, it can take a day or few to resolve or in rare cases up to a week.
Beyond The Immediate Recovery From Cataract Surgery
Once we get beyond the first few days out, the causes of blurry vision after cataract start to narrow down significantly. There are some very common causes and then a scattering of much less common reasons to have blurry vision.
Limitations of the artificial lens
The natural lens inside the eye is responsible for approximately one third of the prescription of your eye. After this lens is removed, it must be replaced with an artificial lens to continue to fulfill this role.
Artificial lens used in cataract surgery; image by Frank C. Müller, CC BY-SA 3.0, via Wikimedia Commons
There are 3 main types of artificial lenses used during cataract surgery
- Standard or basic lenses
- Toric or astigmatism correcting lenses
- Premium, lifestyle or multifocal lenses
Standard lenses are only capable of correcting vision at one focus. Typically after cataract surgery, a power of this lens is selected to optimize distance vision. What this means is that this lens will ONLY focus for distance vision. Your vision will be blurry when trying to read up close. Reading glasses will correct this up close vision. Also check out How To Pick The Best Reading Glasses After Cataract Surgery
In addition standard lenses will NOT correct astigmatism. Any astigmatism you have remaining after cataract surgery will blur vision. Prescription glasses will correct this remaining astigmatism to sharpen up vision.
Toric lenses are an upgrade from standard lenses. These lenses function like standard lenses EXEPT they can correct astigmatism. Thus, when these lenses are optimized for distance vision, you will have sharp distance vision but you will still need reading glasses to see up close.
Lifestyle lenses are designed to correct not only distance vision but up close vision as well. These lenses also come in toric varieties to correct astigmatism. Depending on which lens used, these lenses can get you out of glasses for everything or still require glasses for particular tasks.
Note: certain multifocal lenses will provide a small trade-off between glasses independence and perfect perfect clarity to vision. Rarely one may notice a slight reduction in contrast. But the vast majority don't notice it or aren't bothered enough by it to worry about giving up the freedom from reading glasses.
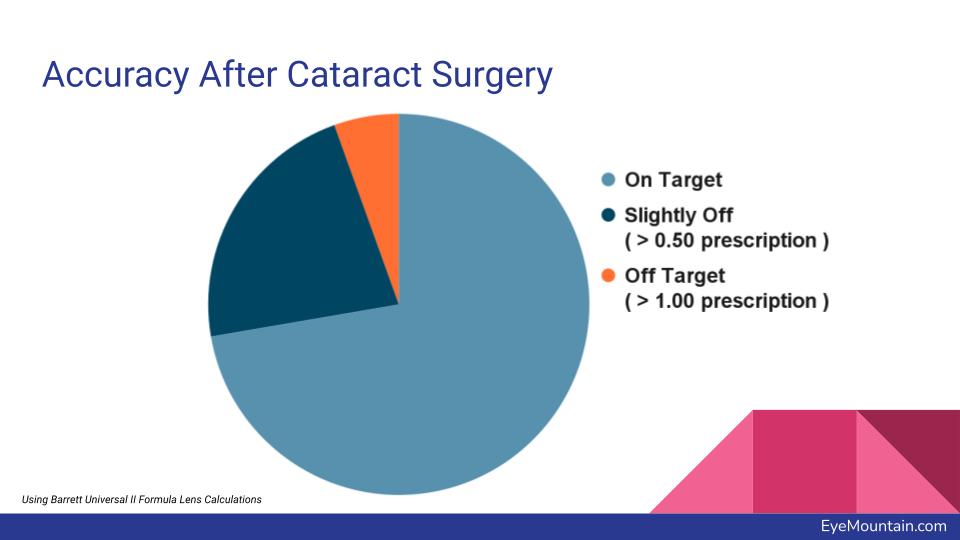
That's how your vision will be with PERFECT calculations. But unfortunately today's technology doesn't allow for everything to always be perfect. This means that some people will end up with residual prescription error.
Residual Prescription
This is by far the most common reason why your vision may be blurry after cataract surgery.
This residual prescription error can cause you to be nearsighted, can cause you to be farsighted or can cause you to have extra astigmatism (even if you happened to get a lens which corrects astigmatism).
The calculations we perform before cataract surgery give us the ideal power of the new artificial lens. But the measurements depend on certain things to be fully accurate. For example, if the new artificial lens sits in a slightly different position in the eye, that will change the prescription! With the best equipment, surgeons and calculations, there are some things which are still beyond our current control.
Because of this, about 5 in 20 patients will have some residual prescription. But of these 5 patients, 4 may or may not notice this extra prescription.
There are certain individuals who are at a higher risk of having residual prescription. The calculations used to calculate the perfect power of lens work best for totally average eyes. However, of course some eyes fall outside of totally average.
- Eyes with highly farsighted or severely nearsighted prescriptions
- Eyes with previous corneal vision correction surgery such as Lasik, PRK or RK surgery
- Eyes with distortions in the cornea, such as those with keratoconus
These particular groups are at a higher risk having residual prescription after cataract surgery.
If you do end up with residual prescription error after cataract surgery, there are a few methods that can correct it. If the prescription is small enough, you may not even notice or be bothered by it. But if you are, glasses are the simplest way (but not the favorite for those individuals looking to get out of glasses with cataract surgery). Occasionally with a toric lens, correcting residual astigmatism may be as simple as having a procedure to manually rotate the lens inside the eye. Rarely a lens may be swapped out for one with a different power. But most frequently, residual prescription error can be surgically corrected with a laser eye surgery procedure such as lasik or PRK. (see also What To Know About A Lasik Touch Up After Cataract Surgery)
Dry Eye
When your eye dries out, this can affect your vision. In particular, this will cause fluctuation of vision.
On the surface of the cornea is a layer of tears called the tear film. This layer protects the cornea from drying out as well as provides essential nutrients to the cornea.
But in addition to that, the tear film actually is the first stop on the passage of light through our eyes. Anything we see must pass through the tear film first before passing through the eye.
When the tear film is good, there are no issues since the tear film will be clear and smooth and conform perfectly to the cornea below.
But when the tear film dries out, we have a different story. The tear film can become irregular and spotty. This scatters light and causes blurry vision.
For many people with dry eye, each blink smooths out the tear film and vision is clear; but a few seconds later the tear film dries out and vision becomes blurry again.
This fluctuation of vision from dry eye remains important after cataract surgery as well and can contribute to blurry vision after cataract surgery.
This is especially true after cataract surgery because one can have more dry eye. There will be extra inflammation from cataract surgery and irritation from the eye drops after cataract surgery. Both of these two things can cause the dry eye to be worse for the first few weeks after the cataracts are removed. Preservative free artificial tears can be helpful to treat this extra dry eye after cataract surgery.
Less Common Causes Weeks To Months To Years Out
After you get past the initial cataract surgery, there can still be changes to your vision. And these changes can happen even despite a completely normal surgery. Your vision may initially be good only to become more blurry later on.
After Cataract
The cataract is suspended within the eye in a bag, called the capsule. When the cataract is removed, this capsule is preserved since its the perfect spot for the new artificial lens to be placed within the eye.
Capsule of eye; image by File:Three Internal chambers of the Eye.png: Artwork by Holly Fischer derivative work: Pixelsquid, CC BY 3.0, via Wikimedia Commons / modified from original
But sometimes, microscopic cataract particles can remain following cataract surgery and these can grow onto the capsule. This causes the capsule to become cloudy. The official term for this is posterior capsule opacification, but it is often referred to as after cataract because it can seem as if the cataract is returning.
This can happen anywhere from months to years out after cataract surgery. But fortunately there is a very easy treatment called YAG capsulotomy which uses a laser to create an opening in that capsule to clear up the vision.
Swelling in the retina
Rarely, residual inflammation from cataract surgery can cause the retina to swell. This typically occurs around the one month mark after cataract surgery. When the retina develops swelling, this leads to blurring of vision.
Fortunately, swelling of the retina is often treated effectively with steroid eye drops to allow the vision to sharpen back up.
Two Severe & Emergency Causes Of Vision Loss
All of those conditions above can cause blurry vision but can be treated over time to restore the vision. And fortunately that makes up the bulk of blurry vision after cataract surgery. But as cataract surgery still is surgery, there are severe (but rare) things of blurry vision which are important to know about.
Infection
Having an infection after cataract surgery, called endophthalmitis, is rare. The risk of infection is roughly 1 out of every 10,000 surgeries. But they do happen.
An infection can occur within the first few weeks following cataract surgery. This leads to blurred vision which can get very severe, increased eye redness and pain.
Be sure to call your eye doctor if you experience a significant drop in your vision in the first few weeks after your cataract surgery.
It is important to treat the infection as soon as possible to prevent the infection from damaging the delicate retina at the back of the eye. This is typically done with injections of antibiotics by a retina specialist.
Retinal Detachment
Within the eye is a jelly-like substance called vitreous; this vitreous breaks down over time and eventually detaches from the retina in the back of the eye. You may notice more floaters in the eye when this happens. And this vitreous detaches more frequently following cataract surgery.
This vitreous may be more firmly attached to parts of the retina. And as this vitreous pulls away, it can tug a hole or tear into the retina.
A retinal tear will cause lots of flashing lots followed by some additional new floaters.
This tear is treated by a retinal specialist who uses a laser to create a barricade around the hole.
But if left untreated, some fluid can get underneath this hole and cause the retina to detach.
Retinal detachments are again an emergency; retinal detachments can cause permanent vision loss. Thus, if you notice a shade or curtain of vision loss, it is important to go to call your eye doctor or go to the emergency room in order to have the retinal detachment repaired.
Summary
Blurry vision after cataract surgery can be stressful, but there are simple causes and solutions for the vast majority of cases. There are some emergencies that are important to know about to prevent you from losing vision in the very rare case it happens. Working with your doctor can help treat this blurry vision and allow you to see your best after cataract surgery.
Like what you just read? Use Social Media?
Stay connected and join the discussion by following Eye Mountain on
Also Check Out: